Introduction
Projects inside the Regenerative Medicine line research:
Guided bone regeneration for the treatment of diaphyseal bone loss of substance. Guided bone regeneration (GBR) finds experimental and clinical applications mainly in dentistry and in peripheral nerve reconstruction. However, the concept of GBR could be useful also in orthopaedic surgery for the treatment of pseudarthrosis and iatrogenic or traumatic bone loss. The use of devices, acting as barriers or regeneration chambers, allows the selective growth of some tissues, blocking the invasion from others which could hinder the healing process. At the same time, the chamber protects and keeps in situ the intrinsic factors essential for the activation of the regeneration processes, so that they can perform their specific activity. The project aims to study the possibility of using GBR in the treatment of diaphyseal bone defects, thorough in situ tissue engineering.
Application of mesenchymal and differentiated cells for cartilage regeneration and study on appropriate scaffolds. The development of biomaterials and scaffolds suitable for cell growth and differentiation is necessary for tissue engineering techniques. For the treatment of cartilaginous lesions, autologous chondrocytes and mesenchymal stem cells are usually employed for preparing engineered constructs. Studies are performed in order to evaluate the efficacy of tissue engineering techniques for the regeneration of acute chondral injuries and degenerative osteoarthritis.
 Repair of bone substance loss with the use of biological or synthetic biomaterials even in presence of stem cells and proteins. Repair of trabecular and cortical bone loss is still a clinical problem and many experimental studies are focused on the evaluation of bone substitutes, alternatively to autologous bone, able to accelerate healing of bone defects and to improve the quality of regenerated tissue. Projects in progress provide the evaluation of biomaterials as scaffolds and fillers for maxillary and mandibular bone, where the amount and the quality of tissue in the implant site is of basic importance for the clinical success. The heterotopic bone formation following subcutaneous or intramuscular implants of biomaterials (with or without biological adjuvant) allows the study of osteoinductive properties.
Repair of bone substance loss with the use of biological or synthetic biomaterials even in presence of stem cells and proteins. Repair of trabecular and cortical bone loss is still a clinical problem and many experimental studies are focused on the evaluation of bone substitutes, alternatively to autologous bone, able to accelerate healing of bone defects and to improve the quality of regenerated tissue. Projects in progress provide the evaluation of biomaterials as scaffolds and fillers for maxillary and mandibular bone, where the amount and the quality of tissue in the implant site is of basic importance for the clinical success. The heterotopic bone formation following subcutaneous or intramuscular implants of biomaterials (with or without biological adjuvant) allows the study of osteoinductive properties.
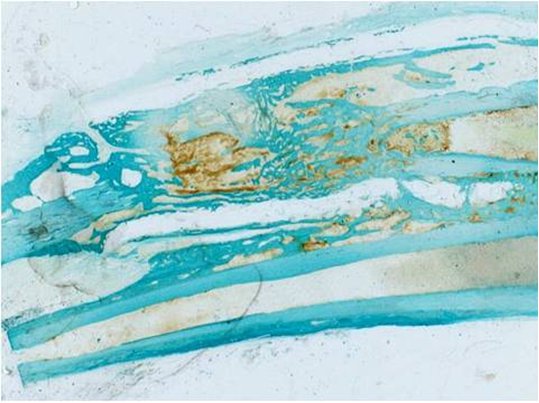
Evaluation of scaffolds for the regeneration of soft tissues of the musculoskeletal system. Tendon injuries still represent a surgical complex problem and current therapies for massive injuries or with loss of substance show important limits. Tissue engineering, through the use of scaffold, growth factors, autologous cells, can represent a good approach. Biological and synthetic biomaterials are studied for tendon and ligament regeneration. In particular, for the development of bioactive scaffolds, biological tissues, such as decellularized matrices consisting of collagen, non-collagenic proteins, growth factors and vascular channels in absence of cells of donors tissue, are investigated. Research projects are in progress in order to develop and test biomaterials and techniques for the treatment of shoulder articular lesions, massive injuries of rotator cuff and other soft tissue lesions.
Preparation and evaluation of biological stimulators in tissue engineering of the musculoskeletal system. Platelet gel (GP) and platelet rich plasma (PRP) are actually largely used, alone or in association with biomaterials or cells, for techniques of tissue engineering and regeneration of musculoskeletal system tissues (bone, cartilage, tendons, muscles). Nevertheless, there are still many controversial aspects about the real efficacy of these platelet derivatives in literature. Methods of preparation, methodology of evaluation and some factors linked to the site of the lesion to be treated seem to be primarily responsible of result variability. For this reason, there are many aspects which need to be investigated to make more reliable and reproducible the advantages linked to the use of growth factors present in GP and PRP. Projects in progress aim to evaluate GP and PRP alone or in association with cells and biomaterials for the treatment of musculoskeletal system pathologies, with particular interest in factors and variables that can have an influence on therapeutic efficacy.