Introduction
Projects inside the General/Traumatological Orthopaedics line research:
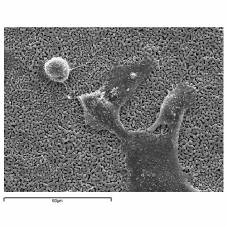 Coating of implant materials for external and internal fixation with bioactive materials to facilitate the process of osteointegration in healthy and osteopenic bone. In reconstructive orthopaedic surgery, many fixation devices are employed; in addition to being biocompatible, they must mechanically and biologically integrate with the bone tissue. Implant surface, the primary stability, the early bone response to the implant, the biological fixation, the mechanical load and the remodeling processes are the principle factors that influence implant osteointegration. Complications related to poor osteointegration of orthopedic implants for fracture fixation are more frequent when biomaterials are implanted in osteoporotic bone because of structural, biomechanical and biological deficiencies linked to ageing and to the disease itself. For these reasons, metal biomaterials with modified surfaces are of great interest in order to stimulate the cellular and tissue response to the implant and, consequently, the success of the reconstructive surgery. Usually, coatings of ceramic or titanium materials are used, with proper morphology and biochemistry to stimulate the growth and bone remodeling. The preclinical evaluation of these devices requires the use of experimental models also of pathological type.
Coating of implant materials for external and internal fixation with bioactive materials to facilitate the process of osteointegration in healthy and osteopenic bone. In reconstructive orthopaedic surgery, many fixation devices are employed; in addition to being biocompatible, they must mechanically and biologically integrate with the bone tissue. Implant surface, the primary stability, the early bone response to the implant, the biological fixation, the mechanical load and the remodeling processes are the principle factors that influence implant osteointegration. Complications related to poor osteointegration of orthopedic implants for fracture fixation are more frequent when biomaterials are implanted in osteoporotic bone because of structural, biomechanical and biological deficiencies linked to ageing and to the disease itself. For these reasons, metal biomaterials with modified surfaces are of great interest in order to stimulate the cellular and tissue response to the implant and, consequently, the success of the reconstructive surgery. Usually, coatings of ceramic or titanium materials are used, with proper morphology and biochemistry to stimulate the growth and bone remodeling. The preclinical evaluation of these devices requires the use of experimental models also of pathological type.
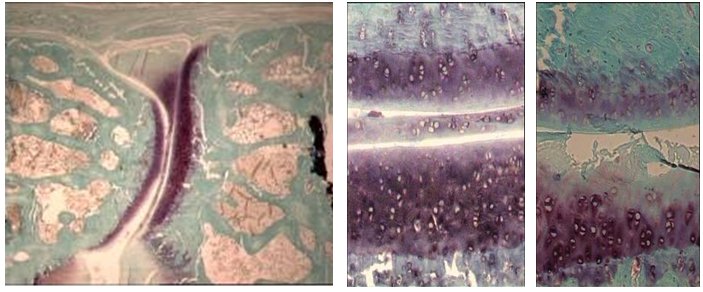 Treatment of traumatic and degenerative joint lesions with biophysical stimulation. Biophysical stimulation with pulsed electromagnetic fields, of appropriate frequency and intensity, has shown to increase in vitro the production of anabolic factors such as TGF-β, BMPs, the synthesis of extracellular matrix (proteoglycans, collagen) and to inhibit inflammatory processes following an increase of adenosine A2a receptors on cell membranes. Studies demonstrated that the stimulation slows down the progression of osteoarthritic lesions to the knee joint and improves significantly the success of surgery using osteocondral autologous graft for traumatic cartilage lesions. The aim of this research is to deep preclinical evaluations on biophysical stimulation, in particular on mechanism of action, modes of application and preclinical therapeutic efficacy compared to other therapies even in association with surgery for cartilage regeneration (id. microfractures, osteocondral transplantations, cell therapies).
Treatment of traumatic and degenerative joint lesions with biophysical stimulation. Biophysical stimulation with pulsed electromagnetic fields, of appropriate frequency and intensity, has shown to increase in vitro the production of anabolic factors such as TGF-β, BMPs, the synthesis of extracellular matrix (proteoglycans, collagen) and to inhibit inflammatory processes following an increase of adenosine A2a receptors on cell membranes. Studies demonstrated that the stimulation slows down the progression of osteoarthritic lesions to the knee joint and improves significantly the success of surgery using osteocondral autologous graft for traumatic cartilage lesions. The aim of this research is to deep preclinical evaluations on biophysical stimulation, in particular on mechanism of action, modes of application and preclinical therapeutic efficacy compared to other therapies even in association with surgery for cartilage regeneration (id. microfractures, osteocondral transplantations, cell therapies).
Stimulation of bone regeneration processes with biophysical therapies. There are different biophysical therapies acting on bone tissue: pulsed electromagnetic fields, ultrasounds, shockwaves. Although there are a number of clinical applications, some aspects on the biological mechanisms of action of biophysical stimulation are still not completely clarified. Some studies are in progress about the therapeutic role of biophysical stimulation for the repair of trabecular bone substance loss, diaphyseal fractures and related complications, implant osteointegration.
o-facciale. A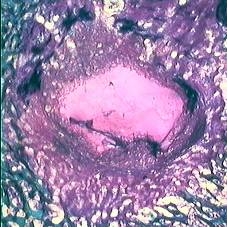 ttualmente, l’osso autologo costituisce il gold standard per migliorare i processi di rigenerazione; tuttavia l’interesse è rivolto anche ai materiali di sintesi aventi caratteristiche di biocompatibilità, osteoconduzione, osteoinduzione e proprietà meccaniche. Scopo delle ricerche in questo settore è la valutazione di nuovi biomateriali sviluppati da esperti nel settore della sintesi e caratterizzazione di biomateriali concepiti per la riparazione delle perdite di sostanza ossee e valutare la traslazione clinica dei risultati.
ttualmente, l’osso autologo costituisce il gold standard per migliorare i processi di rigenerazione; tuttavia l’interesse è rivolto anche ai materiali di sintesi aventi caratteristiche di biocompatibilità, osteoconduzione, osteoinduzione e proprietà meccaniche. Scopo delle ricerche in questo settore è la valutazione di nuovi biomateriali sviluppati da esperti nel settore della sintesi e caratterizzazione di biomateriali concepiti per la riparazione delle perdite di sostanza ossee e valutare la traslazione clinica dei risultati.
Biomaterials for the treatment of bone loss. Bone repair in the presence of bone defects represents an important clinical problem in orthopaedics and maxillofacial surgery. Nowadays, autologous bone is the gold standard to improve the regeneration process; by the way, the focus is also on synthetic materials with characteristics of biocompatibility, osteoconduction, osteoinduction and mechanical properties. The research aims to evaluate new biomaterials to heal and regenerate bone loss.
New biomaterials, porous cement and fixation devices for the controlled release of antibiotic for the treatment of bone infections. Post-traumatic and post-surgical orthopaedic infections still represent a serious complication in the treatment of exposed fractures and prosthetic implantation surgery. Surgical debridement, removal of fixation devices and prostheses, systemic or local administration of antibiotics represent the treatments of choice for these complications. In most cases, the microorganisms responsible are Gram-positive, in particular strains of Staphylococcus, many of which have developed resistance to methicillin and gentamicin. The use of antibiotic-loaded cement spacers and nails 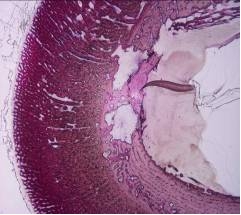 or other resorbable biomaterials also loaded with antibiotics to be used at the site of infection after surgical debridement have been proposed. The aminoglycoside gentamicin, for its chemical characteristics, is considered optimal for a slow release from PMMA. Recently, to face the increasing antibiotic resistance, the use of vancomicin, tobramycin and teicoplanin has been proposed, alone or in association with gentamicin, to load devices in PMMA. The aim of the project is to verify the biocompatibility and biofunctionality of new porous bone cements, that can be loaded, during surgery, with antibiotics alone or in association. This could allow the use of new bone cements in prosthetic implant for the revision of septic prosthesis, or for the construction of spacers or for coating internal fixation means for septic fractures.
or other resorbable biomaterials also loaded with antibiotics to be used at the site of infection after surgical debridement have been proposed. The aminoglycoside gentamicin, for its chemical characteristics, is considered optimal for a slow release from PMMA. Recently, to face the increasing antibiotic resistance, the use of vancomicin, tobramycin and teicoplanin has been proposed, alone or in association with gentamicin, to load devices in PMMA. The aim of the project is to verify the biocompatibility and biofunctionality of new porous bone cements, that can be loaded, during surgery, with antibiotics alone or in association. This could allow the use of new bone cements in prosthetic implant for the revision of septic prosthesis, or for the construction of spacers or for coating internal fixation means for septic fractures.
